

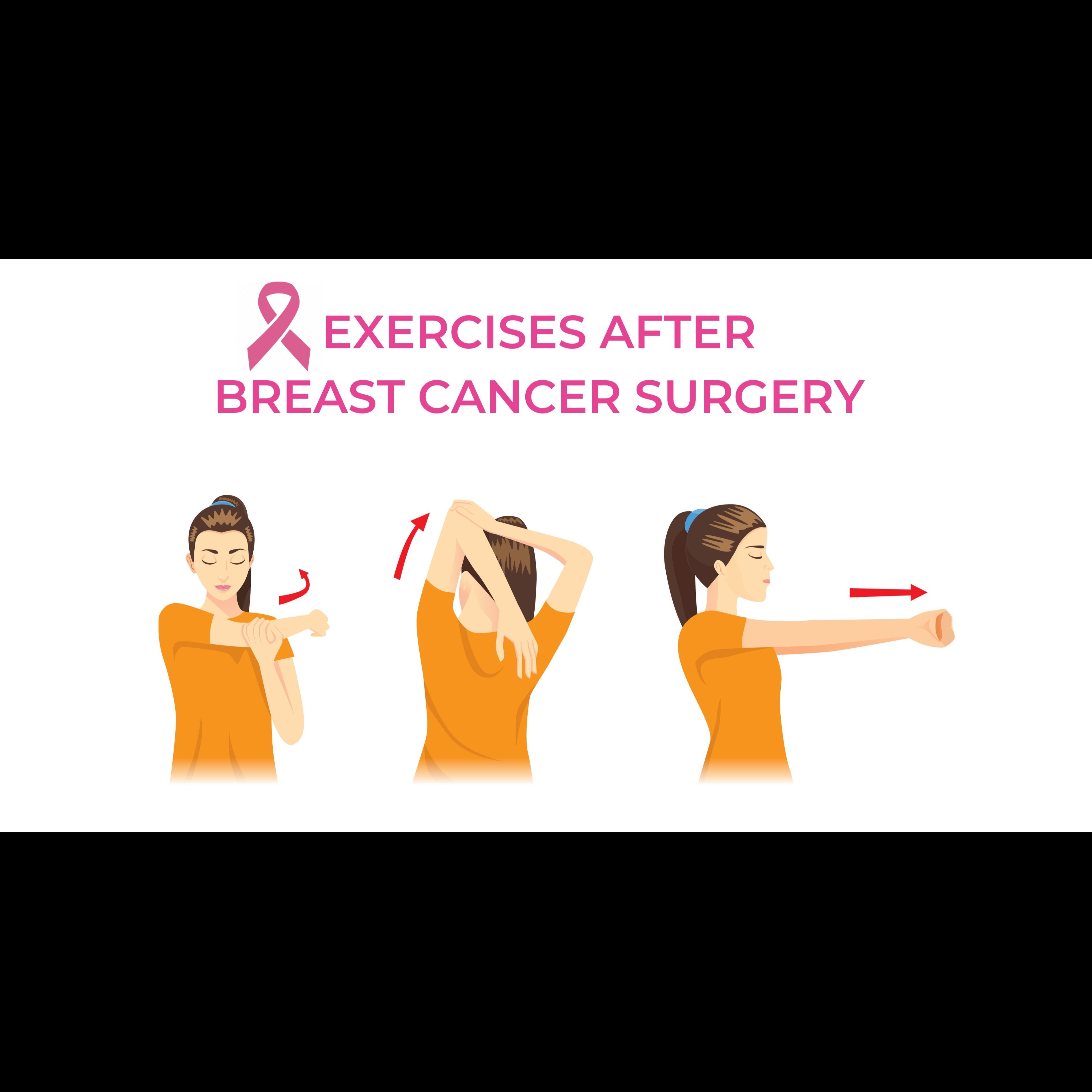

Physical therapy after a mastectomy is essential for regaining arm and shoulder mobility, reducing pain and stiffness, preventing complications like lymphedema and cording, and improving overall physical and emotional well-being. It typically involves a personalized program of exercises, manual therapy, and education, often starting soon after surgery and continuing through various stages of recovery. Benefits of Physical Therapy After Mastectomy Physical therapy offers numerous benefits for individuals recovering from mastectomy: • Restoring Range of Motion (ROM): Surgery can lead to tightness in the chest and armpit, restricting shoulder and arm movement. Physical therapists guide patients through exercises to gradually regain full ROM, enabling daily activities like dressing, bathing, and reaching overhead. • Pain Management: Post-surgical pain, discomfort, and nerve irritation are common. Physical therapists use gentle techniques, stretches, and education on proper movement to alleviate pain and discomfort. • Strengthening Muscles: Weakness in the chest, shoulder, and upper arm muscles can occur due to surgery and reduced activity. Targeted exercises help rebuild strength, promoting functional independence • Lymphedema Prevention and Management: If lymph nodes are removed, there's a risk of lymphedema (swelling in the arm). Physical therapists can provide manual lymphatic drainage, compression therapy, and specific exercises to prevent or manage swelling. • Addressing Scar Tissue and Cording: Scar tissue can form and restrict movement, sometimes leading to “cording“ or axillary web syndrome, which feels like tight bands under the skin Physical therapy includes scar massage and stretching to improve tissue mobility and reduce discomfort • Improving Posture and Body Mechanics: Changes in breast structure can affect posture, leading to back, neck, or shoulder pain. Physical therapy helps correct postural imbalances and educates patients on proper body mechanics. • Psychological Support and Education: Beyond physical recovery, physical therapy provides a supportive environment where patients can ask questions, share concerns, and feel more in control of their healing process. Therapists educate patients on what to expect, how to adapt daily activities, and how to perform exercises correctly at home. A typical physical therapy session involves an initial assessment of mobility, strength, and pain, followed by guided exercises and manual techniques. Patients are often given a customized home exercise program to continue their recovery independently. Common Exercises Examples of exercises commonly recommended include: • Deep Breathing: Helps relax muscles and ease discomfort around the incision. • Shoulder Rolls: Gently stretches chest and shoulder muscles. • Arm Circles (Forward and Backward): Improves outward movement and overall shoulder mobility. • Wall Crawls (Side and Forward): Gradually increases arm elevation and shoulder flexibility. • Wand Exercises: Uses a stick or broom handle to assist in overhead arm movements. • Hands Behind Neck/Back Climb: Stretches the chest and shoulder area, improving range of motion for tasks like dressing. • Scar Massage: Once incisions are fully healed, gentle massage helps soften tissue and improve blood flow, preventing scar tissue limitations It is important to perform exercises slowly, without pain (though a gentle stretch or pulling sensation is normal), and to stop if sharp pain occurs. Pain medication can be taken before exercises to improve comfort. Long-Term Considerations Physical therapy is not just for immediate post-operative recovery; it can be beneficial for months or even years after surgery, especially if radiation therapy is involved, to maintain arm and shoulder mobility and prevent complications like radiation-induced fibrosis. If full arm movement is not regained within 3-4 weeks, or if new symptoms like worsening pain or swelling occur, it's important to inform
We hate spam too.